Coastal Simulation Program team flies to the Central Coast to give onsite training
Not long after simulating a recent trauma scenario with the travelling Coastal Simulation Program team, Dr. Julia Low AhKee and Bella Coola General Hospital staff faced a similar scenario in their emergency department.
“We had a similar patient (motorcycle accident), with pneumothorax, multiple rib fractures, lung contusions, compound tibia-fibula fracture,” says Julia. “So the Sim visit was very helpful. There were lots of practical scenarios, tailored to our small town, rural facility. It would be great to have them come up as much as possible, but twice a year would be good.”
“The teachers also provided us with some great online resources that we can easily implement into our practice. It was a non-confrontational atmosphere, with relaxed teachers, and a healthy learning environment.”
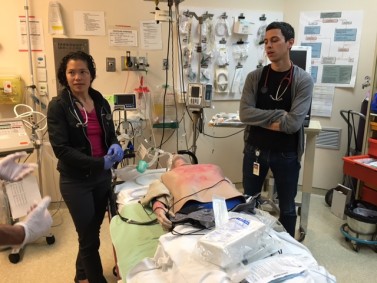
Dr. Julia Low AhKee and Dr. Cal Shapiro at Bella Coola General Hospital are taken through a simulated burn scenario.
The team – Dr. Shannon Chestnut (Medical Education Lead, Simulation), Dr. Hazel Park (Medical Director Regional Trauma Program, LGH Emergency Physician/Trauma Team leader), Karen Schafer (Education Lead, Simulation Strategy) and Dr. Ross Brown (Co-Senior Medical Director/Trauma Surgeon) – travelled with two mannequins (SimJr and an adult full-body task trainer) to the Central Coast earlier this month to provide simulation based Emerg/Trauma education at Bella Coola General Hospital and R.W. Large Memorial Hospital in Bella Bella.
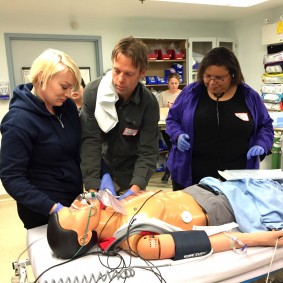
Bella Bella: RN Anne Timothy RN from FNHA in Anaheim Lake, RN Cory Purvis and Dr. Lauri-Ann Shearer get simulation training for a mass casualty boating accident trauma.
Cultural understanding
But that wasn’t the only reason.
“We also went to get a better understanding of the hospitals and community resources and culture,” says Karen. “It was a great trip. We were warmly welcomed and able to have open conversations about all aspects of life at the hospitals and within the community. The teams were strong overall and we came to more fully understand the local culture and barriers and the impact it has on practice and what is possible.”
To encourage more simulation training within their own environment, the team left the adult full body task trainer at Bella Coola General Hospital for staff to continue to use.
“There is enormous value in doing simulation within the environment and with the resources that are available locally,” says Shannon, Medical Education Lead, Simulation. “We were able to facilitate medical learning, but also help identify areas for improvement in systems and department set up that could help in the care of patients in the future. That is the kind of thing that can’t happen out of their practice environment.”

The team – Dr. Shannon Chestnut (Medical Education Lead, Simulation), Dr. Hazel Park (Medical Director Regional Trauma Program, LGH Emergency Physician/Trauma Team leader), Karen Schafer (Education Lead, Simulation Strategy) and Dr. Ross Brown (Co-Senior Medical Director/Trauma Surgeon) – travelled to the Central Coast recently.
Simulation is an interactive learning and practice technique, often using high-tech manikins (in this case SimMan, SimJr. and SimBaby) to create emergency situations or typical patient care scenarios that “simulate” reality in a risk-free environment. It also provides an opportunity to improve systems and processes.

