Renowned North York MD shares lessons learned with Coastal provider
Award-winning health technology expert Dr. Jeremy Theal visited Coastal physicians and clinicians late last month to talk about the benefits of clinical information systems and share lessons learned from multiple implementations.
For Dr. Theal, the key to success is taking the time to involve physicians and clinical leaders.
As chief medical information officer and a staff gastroenterologist at Toronto’s North York General Hospital (NYGH), Dr. Theal led the phased implementation of the eCare project, starting in 2007 and culminating with hospital-wide adoption of a Cerner shared clinical information system in 2015. NYGH is a community teaching hospital affiliated with the University of Toronto with about 124,000 emergency department visits annually and 426 beds.

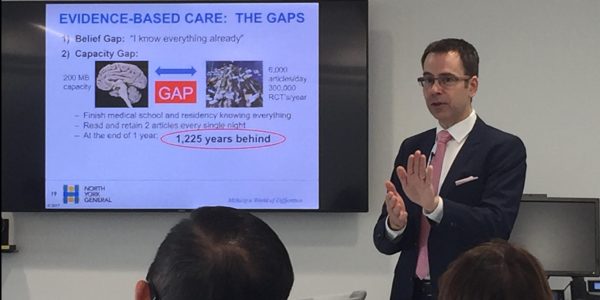
A slide from Dr. Jeremy Theal’s September presentation at Lions Gate Hospital.
All that work to implement eCare was worth the effort, said Dr. Theal, who delivered his presentation at Lions Gate Hospital. “We’re very happy with it.”
(Click here to view the entire presentation.)
He emphasized that implementing a clinical information system should not be considered a technology project for technology’s sake – it must be viewed as a clinical project first and foremost, with the primary goal of improving patient outcomes.
“It’s really about getting clinicians involved that’s going to make a difference.”
Dr. Theal said the temptation to blame the potential adverse effects of using an electronic health record on a particular clinical information system needs to be avoided, because it’s ultimately about the user, not the tool.
“This would be the equivalent of stating that a particular brand of tool from a hardware store was unsafe because an injury occurred while someone was misusing it.”
The NYGH eCare project has won six national awards for innovation, quality and safety for patient care since 2010. Find out more about what helped make eCare a success on page two.
Well-designed systems drive evidence-based care
Implementing advanced clinical information systems is a blood, sweat and tears exercise. So why shouldn’t we just stay on paper? According to Dr. Theal, there’s plenty of evidence to support the change.
- In 2006, when NYGH was using paper-based patient orders, only about 35 per cent of hospital admissions were initiated using an evidence-based standardized protocol. Today, using a computerized provider order entry (CPOE) system, the number is over 97 per cent. This means nearly all hospital admission orders are based on the most up-to-date, evidence-based treatment and studies show this has improved patient safety, clinical practice and even saved lives. Dr. Theal reported that North York’s mortality rates dropped 45 per cent by using CPOE versus paper orders.
- About 6,000 articles are published every single day, and no single physician can keep up. If a system is designed to put the best evidence in front of physicans who are making decisions, then patients will receive the highest level of evidence-based care. “When new information is available, we can have it in our system in under a year,” says Dr. Theal. “If it’s crucial information… we’ve actually had situations where it’s been updated in our system within 24 hours. Try to do that on paper.”
- A clinical information system also enables what Dr. Theal calls an interprofessional approach to care. “It’s not about the lone wolf model of physician practice anymore. It’s about using all the different scopes of practice, expertise and leveraging together as a team to help that patient.”
About Jeremy Theal
Dr. Theal has served as an advisor to more than 80 hospitals and to several public health authorities and private companies in Canada and other countries. He is the physician lead of the Ontario Hospital Information System Adoption and Benefits Team and the 2015 recipient of the Ontario Minister’s Medal Honouring Excellence in Health Quality and Safety.