Special Edition: Ebola preparedness
The Ebola virus has dominated news in recent weeks, with stories of cases and “suspect” cases in the US, Europe and other countries attracting extensive media coverage, speculation and–unfortunately–misinformation.
Firstly, let’s be clear. There are no confirmed cases of Ebola in VCH or British Columbia. Some people have suggested we have some “suspect” cases in Lower Mainland hospitals. Again, this is not the case. Across Canada, there have been a small number of individuals returning from affected African countries who have developed fever and been tested for Ebola. All of these tests have come back negative. Other causes of fever, such as malaria, remain much more likely among returning African travelers than Ebola.
As Chief Medical Health Officer for VCH, I want to reassure all of you that while no Ebola cases have arrived at any of our hospitals, we are ready to handle such a patient in the unlikely event that one might arrive.
Infection Control and Public Health have been preparing for months on how to deal with a suspect Ebola case. Training has been provided for front line staff and will continue to be rolled out over the coming weeks while all family physicians in the region have been sent information about Ebola and management of suspect cases who may present in their offices.
Mask misinformation
It is also important to dispel misinformation about the type of personal protective equipment necessary to handle a suspect or confirmed Ebola patient. Contrary to suggestions by some, evidence shows an N95 respirator is not required for assessment of suspect Ebola patients. Ebola is not airborne so while your personal protection equipment should include a surgical or procedural mask, it does not need to be an N95 respirator. This means fit testing is not required.
Policies and procedures
All our existing policies and procedures can be found on our VCH Connect intranet site. These are consistent with national and international guidelines and I encourage you to take a moment to review them if you can.
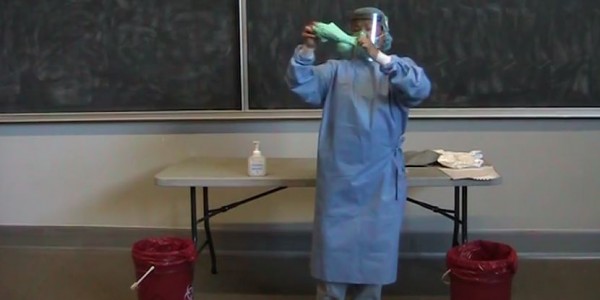
PPE training video
Video is being updated. Please check back.
More information
Further information on Ebola, including information for travelers, including health care workers, who may have returned from Ebola-affected countries is available on the BC Centre for Disease Control website.
VCH, like all health authorities and officials across Canada, is not taking the Ebola situation lightly. We recognize the importance of keeping staff and the people we serve safe. That also means we have a responsibility to provide facts, not speculative or emotive information that might cause undue anxiety.
We will share more on Canada’s approach to Ebola as the national protocols and guidelines are refined. In the meantime, please share your questions and comments below. We can help to support you to be ready to deal with a case in the unlikely event one should arrive in our area.


Mike G
Hello Dr. Daly,
Is there an important distinction to be made between the way a virus is known to spread throughout a population, and how it could be transmitted on an individualized, albeit rare basis? Is disagreement here due to the fact that we have not agreed on our definitions of “direct contact” and “airborne”?
Scientific evidence suggests that Ebola does not spread through the airborne route. Common sense suggests that if a symptomatic patient sneezes, coughs or vomits in the direction of a bed-side care provider, virus may temporarily be suspended in the air that care provider will need to breathe. If I were that care provider I would not really care whether the mechanism of possible transmission at that point is defined as airborne, droplet, or direct contact. I would want 100% confidence that it is safe to keep breathing and continue care.
I note that the Centers for Disease Control in the US has just strengthened its guidelines regarding PPE, specifying no exposed skin, full hoods, and N95 or stronger respirators:
(ref: http://www.cdc.gov/media/releases/2014/fs1020-ebola-personal-protective-equipment.html)
I am very pleased to read about the ongoing training that front line staff in Emergency and Intensive Care units will be receiving on the protocols for donning and doffing the PPE. I hope as everyone else that these remain just preparatory measures to treat the Ebola patient that never arrives.
g bright
Now if the moderator allow views other than the company line ……………………
watch this https://www.youtube.com/watch?v=ahBzAn4w-9M
g bright
Dont let the CDC ” Centyer For Disease Confusion ” try to tell you that EBOLA is not transmittable via airborne droplets ! Our own Candien study showed just that ! So dont go lying to us !i
Clay Adams
As Dr. Patty Daly has already stated, Ebola is not spread by droplets nor is it airborne. That is a fact, not a lie. It concerns and disappoints me when people suggest they are being lied to. Nobody is lying about Ebola or its risks. Why would they? There are health care workers and leaders in VCH and around the globe working hard – often at personal risk – to create safe environments to deal with it and other deadly diseases. People have a right to believe what they believe but whether they choose to believe the facts is up to them. Just please do not confuse ignoring the facts as “lying”. Thanks for taking the time to comment.
g bright
Ebola is air borne use a respirator !!!
Do NOT belive anything from the CDC-” Center of Disease Confusion “
g bright
Ebola is transimissable via droplets .
Health Care wrokers should wear respirators when dealing with Ebola .
Patricia Daly
Ebola is not transmitted by droplets, nor is it transmitted by the airborne route. It is transmitted by direct contact of mucous membranes (eyes, nose, mouth) or broken skin with the blood or body fluids of a patient who is sick with Ebola. Infectious body fluids include blood, feces and vomit. It can also be transmitted by a percutaneous (needlestick) injury with a contaminated needle or sharp.
jim
pls check with Worksafe BC that N95 is not required. we are led to believe we must, legally use them.
Mike G
Dr. Daly, could you please clarify something? The US Centers for Disease Control webpage regarding mode of transmission of Ebola virus includes urine, sweat, and saliva among the bodily fluids which, if infected, could spread the virus to others. While airborne transmission over a distance seems to not be a threat, could not a HCW in close proximity to a heavily symptomatic patient be at risk from fine droplets or aerosol temporarily airborne as a result of the patient coughing, sneezing, or violently vomiting? Shouldn’t the level of protection for HCW’s in terms of masks and other PPG be purposely set higher (ie., N95 face masks, full hoods, etc) considering the high morbidity of the disease and risk it poses to caregivers?
Thank you.
(reference: http://www.cdc.gov/vhf/ebola/transmission/index.html)
John
Thank-you for the PPE training video.. I have a couple of questions.
Why do you use hand sanitizers when hand sanitizers are not effective against viruses? There is no mention of hand washing after finishing the process of disrobing.
Would double gloving give an extra level of protection leaving the inner glove on while removing the potentially contaminated protective equipment?
Patricia Daly
Hand sanitizers are very effective against viruses, and will kill the Ebola virus. Hand washing is also effective and can also be used after disrobing, if a sink is available. The video was shot during a classroom demonstration which is why hand sanitizer was used.
Regarding glove removal, both gloves should be removed at the same time. It would be extremely difficult to try and remove only the outer glove and could lead to further contamination of the inner glove.
The technique for gown and mask removal in the video is designed to minimize the risk of contaminating the ungloved hands during removal, but you will note sanitizing of the hands is recommended after each step and when all steps are concluded as added protection.