Hear one dietitian’s experience with 48/6
In the last year, units across VCH and BC have been implementing 48/6, a structured approach to what we do every day, patient assessments and care planning. Since 48/6 has changed some of the ways teams work together, we wanted to hear how it’s being implemented, how it’s improved collaboration and about some of the challenges along the way. So the other week we talked to Angel a dietitian on Richmond Hospital’s 2 south to hear about her experience with 48/6.
What was the key to successful implementation on your unit?
“Our team is really tight and the successful roll out and implementation is attributed to all of them,” said Angel. They’ve gone a step further and integrated 48/6 into their daily workflow. “During our daily rounds our PCC wraps up every single patient by asking if there was anything identified in 48/6.” Angel said this helps nursing stay on top of the assessments and gives the allied teams a heads up when consultations are required.
How has 48/6 improved communication?
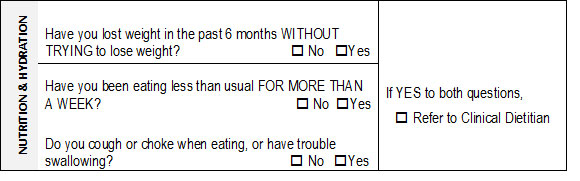
1. It encourages conversations about nutrition
“Nutrition is everyone’s responsibility in a hospital setting.” said Angel. Dietitians rely on nursing to provide them with insights that can only be gathered at the bedside. “The 48/6 screening questions have helped highlight nutrition priorities for the team and trigger conversations when issues arise.”
2. It improves after-hour communications
“I work on the unit part time from Monday to Friday so the interdisciplinary care plan has really helped me communicate specific dietary instructions to staff and physicians, who work after hours, because all the instructions are consolidated as key points in one area.”
3. It provides a holistic picture of patients
Angel says that having the ability to access all of the pertinent information for a patient in the care plan has really helped them see the bigger picture. For example when a patient has a positive screening for multiple functional areas, such as nutrition, mobility and medication management, social work asks what if these issues are related to the support they got at home before they were admitted. If support was the issue, social work can proactively work with the patient to find more support on discharge.
Were there any challenges?
With every new change come a few challenges along the way. For Angel, her challenge was an initial increase in workload. “At the beginning I received quite a few inappropriate referrals, which made it hard to keep up with my regular workload. But now after a few months of working together as a team, getting used to the questions and understanding when to refer, nutrition concerns are being highlighted earlier in the admission process and the number of inappropriate referrals have decreased.”
Where are we at with 48/6 today?
48/6 was implemented in 2014 across all of the Richmond and Coastal communities of care. It is currently being implemented in Vancouver where implementation will be complete by July 2015.
Have a story to share or questions?
Email Sue Goulding, 48/6 project manager at: Sue.Goulding@vch.ca or post your questions in the comments field below.
About Angel Luk
Angel has been at VCH for three years and has worked in a number of settings including, Trauma, ICU and Burns and Plastics. She currently works on 2 South at Richmond Hospital where she works primarily with telemetry inpatients and outpatients.
Learn more about 48/6
The goal of 48/6 is to improve patient care, maintain pre-hospital level of independence, and address issues identified through the screening process. Visit our pages on VCH Connect to learn more.