LGH researcher co-authors study that places 19th in Discover Magazine’s Top 100 science stories of 2015
Just getting noticed by Discover Magazine was a thrill in itself for Dr. Robert Tarzwell, Lions Gate Hospital’s Clinical Research Director – Mental Health. For a history-making brain scan study he co-authored to be selected #19 of the respected science magazine’s top 100 stories of 2015, however, has left him “beyond excited.”
“We were pleased simply to be noticed by Discover, and to be considered one of the 20 most important science stories of the year – we came #19 of 100 – is really an almost indescribable thrill and certainly a career highlight,” says Robert, a Clinical Assistant Professor in the Department of Psychiatry at UBC and a specialist in both psychiatry and nuclear medicine.

Dr. Robert Tarzwell calls the Discover Magazine ranking of the brain scan study “a career highlight.”
Robert was invited by U.S. researchers from UCLA and Amen Clinics International to co-author the largest brain scan study in history – 21, 143 subjects.
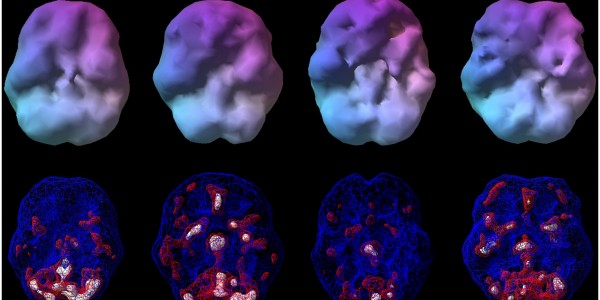
The study, “Functional Neuroimaging Distinguishes Posttraumatic Stress Disorder from Traumatic Brain Injury in Focused and Large Community Datasets,” demonstrates how brain perfusion single-photon emission computed tomography (SPECT) images accurately distinguish PTSD from TBI when compared against healthy controls and also against cohorts with a high burden of psychiatric disease.
Research should benefit combat veterans with PTSD and TBI
While PTSD and TBI patients have overlapping symptons – amnesia, insomnia, irritability, reduced frustration tolerance, and low mood and energy – treatments are very different. With the ability to distinguish between the two disorders, clinicians will now be able to tailor treatment to the individual for better health outcomes. The research is particularly useful for combat veterans, who frequently suffer from both PTSD and TBI.
“In situations where PTSD and TBI coexist, we want to avoid treatments for one condition which could slow down recovery of the other condition,” Robert explains. “For instance, it is very common to use sedatives in PTSD. These are very unhelpful in TBI, because they only exacerbate the main problem: under activity in the central nervous system. However, we also know from survey data that possibly as many as two thirds of individuals with PTSD and TBI do receive sedative medication as part of their treatment.”
Doc credits LGH’s nuclear medicine and psychiatry departments for his success
Robert credits much of his success in this research project to the special working relationship forged between the departments of psychiatry and nuclear medicine at Lions Gate Hospital, as well as the hospital’s Foundation.
“The foundation provided the functional brain imaging equipment and the department of psychiatry has worked together with nuclear medicine in referring complex, treatment resistant cases to our functional neuroimaging program. This allowed me to acquire the skills and expertise to make a meaningful contribution to this study.”
Click here to watch a short video on the study.
On the heels of the successful US study, Robert is currently working on a new study using LGH data. He’s collaborating with Dr. Cyrus Raji and Dr. Dan Silverman of UCLA on a study looking for differences between unipolar depression and bipolar depression with LGH data, sponsored by the Canadian Bipolar Foundation. The study will be completed in 2016.