Medical Assistance in Dying
Vancouver’s All-Staff Forum considers thoughtful and respectful approach to topic
**To view the forum, click the webcast link. Forum materials will be posted on the One Vancouver intranet site shortly. Policy, process and forms available on VCH Connect.
What would you say if a patient or client asked you about Medical Assistance in Dying? This conversation isn’t a simple one, and for some, a very sensitive topic that represents a shift in the historical view of healthcare.
“Patients are much less afraid to talk about their condition, and dying, than we might be,” advised Dr. Peter Edmunds, regional medical director of home, community and palliative care. He shared further: “This opens the conversation to talk about a patient’s condition and its trajectory, about treatment options, including pain management. Provision of medical care does not stop while exploring Medical Assistance in Dying with a patient.”
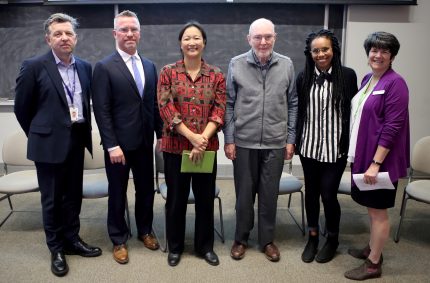
All-Staff Forum panel: Dr. Peter Edmunds, Darren Kopetsky, Dr. Kushner-Kow, Dr. Terry Anderson, Rachel Ricketts, Leighanne MacKenzie
Dr. Kushner-Kow, a Vancouver physician, shared her experience working through the Medical Assistance in Dying process with patients. She has supported patients who have requested the procedure, with some following through to death, and others choosing other paths of treatment for their condition. She encouraged staff not to be afraid of the request form, and echoed Dr. Edmunds in the fact that care continues despite this request, and that a full assessment process is yet to come after the request form is completed by a patient.
“Overall, my experience has been positive — as staff and physicians, we’re still anxious about it, but everyone has been so willing to help each other,” shared Dr. Kushner-Kow. “Medical Assistance in Dying is definitely not treated as ‘just another surgery or procedure.’ There is great acknowledgement of this being special, with the patient and staff taking the time they need, and supporting each other.”

Featured Speaker – Darren Kopetsky, Facilitator – Leighanne MacKenzie, panelist Dr. Kushner-Kow
Darren Kopetsky, VCH’s regional director of client relations and risk management, and keynote speaker at the event shared VCH’s policy and process with the packed auditorium of 250 staff and physicians at VGH, and another 300+ joining via webcast at six facilitated satellite sites, as well as individually or in small groups. In presenting the topic, Kopetsky asked staff to consider their own view of Medical Assistance in Dying and respecting each other’s beliefs. While Medical Assistance in Dying is federally legislated, each health authority defines its own policy and process, which varies across the province.
“Staff should give consideration to Medical Assistance in Dying, and be aware of their own situation related to providing this treatment for patients,” said Kopetsky. “With prior knowledge, supervisors can not only plan around scheduled staff, but also be prepared to support staff around the circumstance of Medical Assistance in Dying.”
VCH policy does not insist that staff in disagreement with Medical Assistance in Dying must participate. This new area of care does require that staff respect the individual decisions made by patients. Rachel Ricketts is a CEAN member, and an advocate for Medical Assistance in Dying since her mother made the life-ending decision last year to refuse all food and water, prior to Medical Assistance in Dying being officially legislated.

Panelists Rachel Ricketts (CEAN member) and Dr. Kushner-Kow
“In our case, judgment by others made the painful process even more difficult than it needed to be. While death is a hard topic, it is not the worst-case scenario,” shared Ricketts of her mother’s experience in 2015. “I just ask people to open their hearts, and check their judgments at the door.”
All-Staff Forum Q&A will be posted shortly in VCH News. Staff requiring support around this or any other personal issue are encourage to contact the Employee & Family Assistance Program, or their VCH Spiritual Care Leader. Visit VCH Connect for further information, forms and links.


Marion Wittmann
I am so glad that Medical Assistance in Dying is finally legal in Canada. I hope some day we will also find a way to help those who cannot verbally express this wish to die with some kind of dignity. Having worked for years in geriatric psychiatry it pained me having to help keep people alive who suffered from dementia combined with depression for example who kept pulling out their IVs for hydration only to have them reinserted or have a PEG tube placed. I wish there was an independent ethics committee to support families struggling with decisions for their loved ones who may not get better and are suffering.