VGH ED staff ask & answer, “What matters to you?”
One June 19, VGH Emergency Department participated in its first official “What Matters to You?” Day. On that day, we encouraged all staff to actively ask patients what was important to them. The idea was shared to the Emergency Department from our leadership team: Lara Gurney, Nurse Clinician; Susan Harrison-Salt, Nurse Educator; Lori Quinn and Sarah Turner, Head Nurses.
Staff testimonials
Nicole K, Emergency Nurse: It's so easy to become focused on task management.
I find that taking even two minutes to keep my patients and their families in the loop, letting them know what they’re waiting for, and reassuring them that someone is looking out for them saves a lot of angst. Aside from improving their experiences overall, I really think that making concerted efforts to consider ‘what matters’ most to my patients makes my job easier and saves time in the long run. Happy patients, happy nurse!
Lori Korchinski, Patient Services Manager: I want you to thrive and grow
One thing that we do have control of is our relationships with people- especially our patients.
I know my perspective is a little different as I don’t take care of patients but what matters to me is that I want you to thrive and grow. I hope that I can do the best with what I have to make this ED a great place to work and that you can be proud of the care you provide and it’s my role to support you to do this.
Andrea G, Emergency Nurse: We could relieve some anxiety of those people waiting at triage
For example, how many times do we walk past patients, or family members, and avoid eye contact? How many times do we close the curtain, simply so people will stop staring at us? At triage, how many times do we get busy with the tasks of the job and leave people waiting to check in without even acknowledging them?
I am working on June 19, and I encourage you to join me in acknowledging those patients and family members we so often avoid. We could relieve some anxiety of those people waiting at triage, by simply looking out and saying, “We see you there, and will be with you shortly.” Instead of walking past, and not making eye contact, stop, acknowledge, and find out what is important to them.
Monique McLaughlin, Nurse Practitioner: It is 4 am in Gondar, Ethiopia.
I have spent the last week teaching the nurses here in Gondar, Ethiopia and spending time clinically with them at the University Hospital and the question of what matters to me has certainly given me much to think about. Being here with the constraints of an impoverished society, lack of medical supplies, a patriarchal health care team has certainly made me SO GRATEFUL for the privileges that we have with our Canadian health care system – not only having access ourselves but working within it. What I have realized though that no matter where you are in the world, people who gravitate to health care do so because what matters to them is to serve and give back to our communities and to provide compassionate care. I have always felt that disease itself has no discrimination because it doesn’t matter what your economic, religious, sexual orientation, culture is – people get sick and people either get well or die.
Thank you for giving me this chance to reflect on what matters to me – with the sound of the call to prayer in the background – what matters to me is the human connection that we have an opportunity to exhibit every day in life – it is in the connections that we make with our patients and their families; it is the connections that we make with our work family; it is our personal connections that support and fuel the work that we do. I am grateful for all of you in taking the time to remind us all to always keep central to our practice what matters to you!
Dr. Chad Kim Sing, Medical Director: Many of you helped care for my dad before he passed away.
I really appreciate the occasions when I find enough time to really connect more with a patient and their loves ones. It’s in the “how” I interact with them as well as the “what” I say. You can see it in their faces and body language when they know they are in good hands in our ED, can trust us, and understand what is happening amongst all the chaos of the ED.
I can speak from the perspective of family of a patient who needs family to help advocate.
Many of you helped care for my dad before he passed away in 2015. For this, my family and I will always be grateful. He had a number of health concerns that stemmed from an intracranial bleed while on warfarin that required an emergent craniotomy and subsequent deficits for which my mom learned how to manage (trach, G tube, meds, complete lifestyle changes).
My Dad had many, many admissions to VGH on many services. His pathway into the system was pretty much always via our ED. He always showed strength, courage and determination despite setbacks to get better and always told us “get me home.” As I’m sure we all know, being on the receiving end of the health care system is very different and really quite nerve racking, even despite knowing the system. Sometimes knowing too much sucks.
What matters to me regarding patient care is creating the opportunity and time to show concern and find out how I can help make things a bit better for the patient and alleviating at least some of their anxiety and concern for coming to our ED, even if we don’t always have the answers. It also means respecting their concerns and values too. And it means putting ourselves in their shoes, if only for that period of time we have with them. Sometimes it’s harder to do than it sounds, but this is when I think I am doing a better job.
Scott M, Emergency Nurse: Put your own spin on it.
A few ways the question
“What matters to you?” could be asked are:
“What can we do to support you today?”
“What are your goals in coming to the hospital today? What do you want to achieve?”
“What do you need?”
“Is there anything else you want to tell me that we haven’t talked about?”
Put your own spin on it, make it your own. Asking “What matters to you?” can make all the difference in the type of experience a patient and family may have in the hospital.
Eleanor C, Emergency Nurse: Create as many moments of positivity as I can
For patients, for colleagues, for ourselves, this workplace needs as much positivity as it can get. And that doesn’t mean cheerfulness, it’s more approaching every situation with “How could I make this situation a little better?” By grabbing BW with a line to save time and a poke, by providing knowledge, by listening, by a process of meeting people where they are at in their crisis and finding something that will bring a little levity. It can be as easy as sharing a joke with a patient to put them at ease, letting someone know what they are waiting for, thanking a colleague for being awesome. It can be just a brief moment but those are what create the experience of getting through an emergency.
Yarrow R, Emergency Nurse: An idea we can carry forward into everyday practice
Working in the ever busy Emergency Department I have found that what matters to us as healthcare providers and what matters to our patients can be at real odds. We may make it through the entire visit and not ever be aware of this discrepancy, and therefore we miss opportunities to meet patient’s needs. And if so, aren’t we more likely to see these people for repeat visits, or leave them feeling unheard or unsatisfied? All things that we would likely prefer to avoid.
Thus I love this idea of coming together as a staff and making a concerted effort to ask and therefore have an opportunity to address the things patients and their families’ state really matters to them. Hopefully an idea we can carry forward into everyday practice.
Josh D, Emergency Nurse: Arming patients with information is important
For me, arming patients with information is important. During a quick interaction, you can inform patients about what they can expect during their hospital stay. While it can take extra time when you’re busy, it has the benefit of giving patients realistic expectations. Explaining some of the process and reasons for wait times can go a long way in preventing them from feeling neglected while they are waiting.
How did we prepare?
We reached out to our staff in our daily huddles, and through word of mouth, posters, stickers, and a Facebook page. As well, we did 2 weeks of advertising in our weekly educational tidbits newsletter. The first week focused on “improving our ability to listen” and the second week we focused on “asking the question.” These simple techniques gave staff tools to effectively communicate as well as obtain a deeper understanding of what their patient is experiencing.
We then approached our mentorship group of nurses to spread the word as well.
Staff members then sent out emails to the Emergency Department staff group on “what matters to them” as they began to reflect on June 19.
In conclusion
June 19 was a success! Taking a few minutes to engage is the foundation of patient-centered care.
Please contact us for any question or concerns you may have. We all reflected on how we practice and agreed spending a few minutes to understand each other, even in our chaotic environment, goes a long way in providing patient centered care and mutual respect. You can reach Lara Gurney at lara.gurney@vch.ca and Susan Harrison-Salt at susan.harrisonsalt@vch.ca.
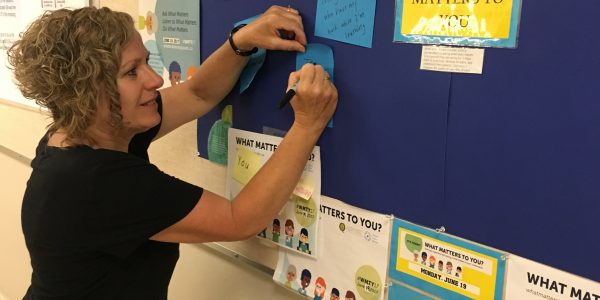
- Becca Sornensen writes what matters to her.
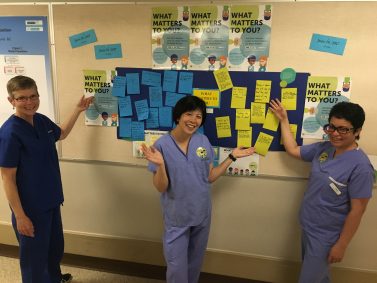
- Cathy Wand, Veronica Tsang, and Vangie Portillo strike a post in front of the VGH ED “What Matters To You?” board
- Susan Harrison Salt and Helena Chan.
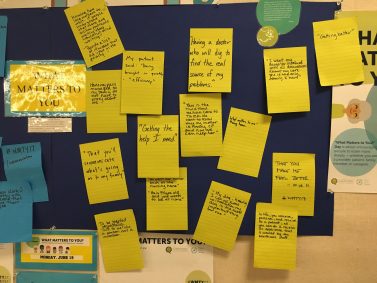
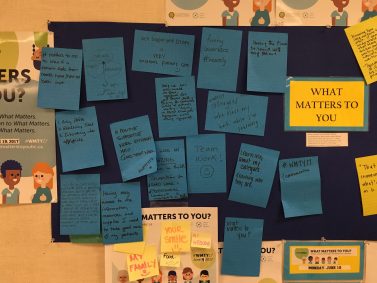
- Patient responses to the question, “What matters to you?”
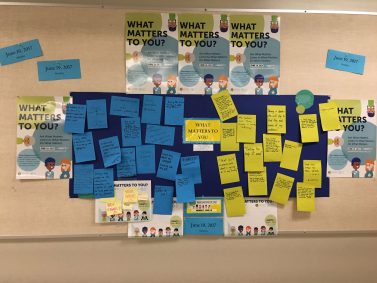
- The VGH ED “What Matters to You?” board.
- Staff share what matters to them.