ICU makes a clean sweep
Live with clutter long enough and you clean forget how cluttered your environment really is. But imagine seeing your environment through others’ eyes. What would you see? And would you like what you saw?
That’s what Kathy Weglo wondered.
“Everyone wants to take pride in their workplace,” says the ICU clinical nurse educator (CNE) at VGH. “But when we asked ourselves what our unit looks like from the outside, from the perspective of families, visitors and patients, we knew we had to roll up our sleeves.”
The ICU embarked on its mission to declutter in March, as one of six VGH units participating in Wave 3 of the CDI Initiative. Hospital-acquired infections like C. difficile can mean the difference between life and death — especially in an ICU. Preventing patients from acquiring a CDI also frees beds for patients in need.
Since launching the CDI Initiative in September 2012, the average number of CDI cases on VGH units has dropped from 5.45 to 4.29 cases per week — an overall reduction of 21 percent. And an achievement the ICU has had a hand in.
Decluttering could save lives

At the bedside: Oversupplied and overburdened bedside carts represented a potential waste of more than $3,000.
“Decluttering isn’t a job for just one person,” says Kathy. “It takes teamwork and I was fortunate to have keen champions willing to engage and represent their peers.”
Robert Bowlby, RN, is one such champion. He consulted with his bedside colleagues on how to limit clutter at the bedside and the results, he says, could save lives.
“Limiting supplies at the bedside was probably the biggest adjustment, but the change I’m most proud of,” says Robert. “Today, we take only what we immediately need to the bedside, which benefits patients.”
Decluttering has reduced the time needed to strip, clean and prepare ICU beds, explains Robert, so in Code Blue or other emergency situations, patients can be admitted even faster.
“Where seconds can mean saving someone’s life,” he adds, “fewer hospital-acquired infections means a quicker response to patients — it’s much simpler when you only have to perform hand hygiene before entering a bed space, rather than donning gowns and gloves when patients are in isolation.”
Reducing waste and saving money
Decluttering will also help the ICU minimize waste and save money — big money.
“Providing best care is our first concern, but keeping a clutter-free and clean environment has the added benefit of reducing waste,” Kathy says.
Limiting supplies at the bedside carts is just the beginning. Improving storage and removing unnecessary shelves and cabinets, where valuable supplies could “disappear,” were important, too.
Add it all up and Kathy estimates the ICU could save more than $140,000 per year by using supplies more thoughtfully and avoiding accumulation of, well, stuff — everything from binders, to pillows to obsolete materials and equipment. During their initial clean sweep, the ICU filled up nine and a half bins and 21 media boxes with garbage, recyclables, VCH tapes and more.
Keeping up the good work
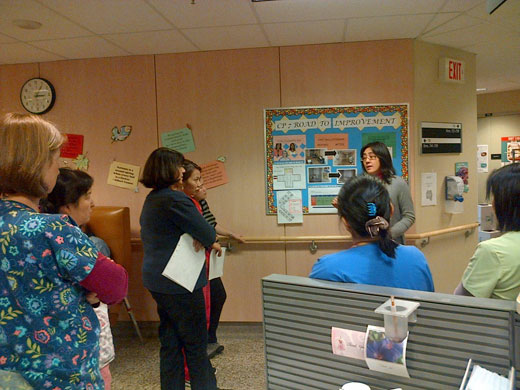
Maintaining momentum: Weekly huddles help keep infection control top of mind and units CDI-free for months at a time.
Since decluttering, the ICU has gone as long as seven weeks CDI-free and nine weeks MRSA-free. In August, the ICU team achieved an 84 percent hand hygiene rate — their best ever, and another example of the unit’s progress. To build on their achievements, Kathy will continue engaging staff and keeping infection control top of mind through regular team huddles.
Doris Bohl, CNE for Subacute Medicine, can attest to the power of huddles. “Staff see how much CDIs devastate patients and they recognize the cost of longer hospital stays,” she explains. “They want to be part of the solution and because they know a patient’s history, they can help us problem-solve quickly and effectively.”
Doris leads weekly huddles to review rates, transmission prevention and, if necessary, discuss positive cases. The results speak for themselves. At the time of publication, units on CP7 were 17 weeks CDI-free; CP10 is now nine weeks CDI-free.
“I’m really proud of our team and the difference they’ve made and can still make,” says Kathy. “We’re determined to keep up the good work and with the continued support of Infection Control and our partners in care – including Aramark and FMO – I’m confident we’ll succeed.”

